The neurodevelopmental illness known as attention-deficit/hyperactivity disorder (ADHD) is marked by recurrent patterns of impulsivity, hyperactivity, and inattention that severely hinder functioning in a variety of spheres of life. All age groups are affected, and symptoms frequently last throughout maturity. ADHD can have a significant negative influence on social, vocational, and academic functioning, which can affect relationships, work, and general quality of life. Despite the fact that ADHD is a complicated disorder with many underlying causes, people can effectively control their symptoms and enjoy satisfying lives by using effective management measures, which may include medication.
A key component of treating ADHD is medication control, which helps many patients achieve better functional results while also relieving symptoms. But for patients, caregivers, and medical professionals alike, sorting through the plethora of prescription options and maximizing care can be difficult. In addition to discussing existing treatment choices, selection criteria, and techniques for maximizing treatment success, this article examines the state of medication management in ADHD.
Understanding ADHD Medications:
There are two main types of ADHD medications: stimulants and non-stimulants. For ADHD, stimulants—like methylphenidate and amphetamine-based drugs—are the most often given and researched pharmacological therapies. These drugs function by raising the brain's concentrations of the neurotransmitters norepinephrine and dopamine, which improve focus, attention, and impulse control.
Those who cannot take stimulants or do not respond well to them may find an alternative in non-stimulant drugs such as atomoxetine, guanfacine, and clonidine. Usually, the norepinephrine or other neurotransmitter systems linked to ADHD are the focus of these drugs.
Selecting the Appropriate Drug:
A patient's symptom profile, comorbidities, drug tolerance, and preference must all be carefully taken into account when choosing the best medicine for a person with ADHD. In order to determine the kind and severity of ADHD symptoms as well as any comorbid disorders that can affect treatment choices, healthcare professionals must perform a thorough evaluation.
Because of their well-established effectiveness and comparatively quick beginning of action, stimulant medicines are often the first-choice treatment for a large number of patients. Nevertheless, individual responses to stimulants can differ greatly, so the best medicine and dosage may need to be determined by trial and error. To customize treatment to the patient's demands and lifestyle, factors like the duration of action, dose schedule, and formulation (e.g., immediate-release vs. extended-release) should also be taken into account.
Non-stimulant drugs provide an alternate therapy option when stimulants are contraindicated or ineffective. The selective norepinephrine reuptake inhibitor atomoxetine has been shown to be effective in lowering symptoms of hyperactivity and inattention in both adults and children with ADHD. Furthermore, to treat the symptoms of ADHD and related deficits, alpha-2 adrenergic agonists such guanfacine and clonidine can be used as supplementary therapy or as monotherapy.
Improving Therapy Results:
More than just writing a prescription is needed to maximize treatment outcomes for ADHD; a thorough, multimodal strategy that takes into account the disorder's complexity is needed. Behavioral therapies, psychoeducation, and supportive techniques are essential in treating symptoms and enhancing functional outcomes in addition to medication.
Behavioral therapies can assist people with ADHD improve their organizational skills, social functioning, and coping mechanisms. Examples of these interventions include parent training programs and cognitive-behavioral therapy (CBT). By addressing underlying issues with executive functioning, emotional control, and interpersonal interactions, these therapies supplement pharmaceutical treatment.
Psychoeducation, which teaches patients and their families about the nature of the condition, available treatments, and coping mechanisms, is another crucial aspect of managing ADHD. Teaching patients about their illness promotes self-awareness, lessens stigma, and gives them the power to actively choose their own course of treatment.
Time management skills, adjustments to the job or school setting, and other supportive strategies can lessen the impact of ADHD symptoms on day-to-day functioning. Developing a welcoming atmosphere that understands and meets the special requirements of people with ADHD can improve treatment compliance and general wellbeing.
Obstacles Things to Think About:
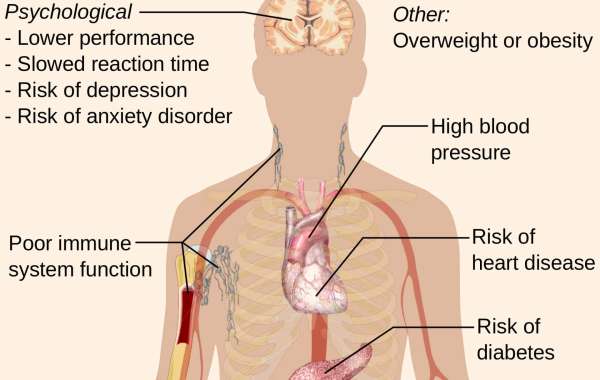
Even though managing medication can be quite successful in reducing symptoms of ADHD, there are risks and difficulties involved. Reduced appetite, sleeplessness, and irritability are common side effects of stimulant drugs that may need changing prescriptions or dosages. Sedation, vertigo, and gastrointestinal problems are among the adverse effects of non-stimulant drugs.
Furthermore, there is continuous discussion and disagreement about the long-term safety and effectiveness of ADHD drugs, especially when it comes to young people. Many studies have shown the short-term advantages of pharmaceutical treatment, but long-term effects on growth, cardiovascular health, and mental health outcomes are still unknown.
In order to evaluate treatment response, keep an eye out for side effects, and modify the treatment plan as necessary, medication management also calls for routine monitoring and follow-up. In order to maximize treatment success while lowering risks, healthcare practitioners must cooperate, address worries or misconceptions regarding medication, and maintain open communication with patients and their families.
Conclusion:
medication management is an essential part of treating ADHD since it helps many people's functional outcomes and relieves their symptoms. With a wide range of pharmacological choices at their disposal, medical professionals can customize treatment regimens to each patient's specific requirements and preferences. But effective treatment of ADHD calls for a multimodal, all-encompassing strategy that incorporates behavioral treatments, psychoeducation, and supportive techniques in addition to pharmaceutical medication. Through careful consideration of available options and collaborative optimization of therapy, people with ADHD can more effectively manage their symptoms and flourish in a variety of spheres of life.